Abstract
Background Previous studies have reported that a combination of Homoharringtonine (HHT), a plant cytotoxic alkaloid derived from the trees of the genus Cephalotaxus, plus intensive chemotherapy (IC) improved the clinical responses of acute myeloid leukemia (AML). Azacitidine (Aza), a DNA hypomethylation agent, has been a "backbone" for novel combinational therapies. In this trial, we assessed the efficacy and safety of adding Aza to HIA/HDA regimen in previously untreated young or eligible for IC patients with AML.
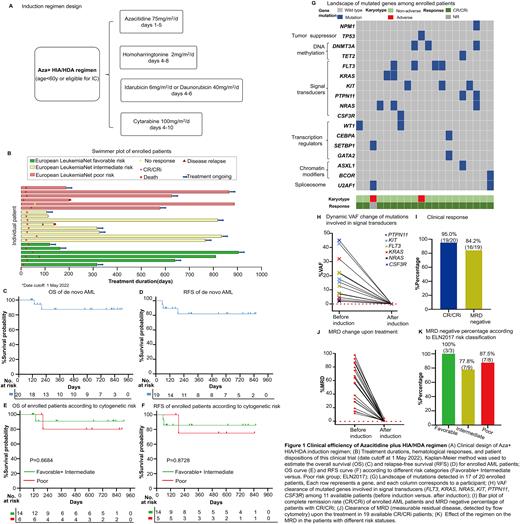
Methods This is a single-center, phase 2 trial (ClinicalTrials.gov: NCT04248595). Aza (75mg/m2/d on days1-5) administered in combination with HIA/HDA [HHT 2mg/m2/d on days 4-8, idarubicin 6mg/m2/d or daunorubicin 40 mg/m2/d on days 4-6, and cytarabine 100mg/m2/d on days 4-10] regimen for patients age<60 or eligible for IC (Fig.1A) The primary endpoint was the composite CR. Secondary endpoints were overall survival (OS), relapse-free survival (RFS), and adverse events (AEs). A leukemia targeted-exome-seq panel including 58 genes and leukemia 47 fusion gene panel were used for screening.
Results Between Aug, 2019 to May, 2022, a total of 20 de novo AML patients were enrolled. The CR/CRi was achieved in 95.0% (19/20) (Fig. 1B). 94.7% (18/19) reached CR/CRi after the 1st cycle of induction therapy and the median time was 25.0d (IQR, 21.0 to 27.0). The median follow-up was 628 days (range, 107 to 905) and the median OS and RFS were not reached (Fig. 1C& 1D). The estimated 2-year OS and RFS were 87.4% (95%CI, 58.1% to 96.7%) (Fig. 1C) and 82.0% (95%CI, 53.1% to 94.0%), respectively (Fig. 1D). No survival difference was observed between the favorable and intermediate versus poor-risk groups in both OS and RFS (Fig. 1E& 1F). Meanwhile, the estimated 2-year OS and RFS possibility of the favorable and intermediate-risk group was 90.9% (95%CI, 50.8% to 98.7%) and 80.0% (95%CI, 20.4% to 96.9%), respectively (Fig. 1E& 1F). While the estimated 2-year OS and RFS possibility of the poor-risk group was 85.7% (95%CI, 33.4% to 97.9%), and 75.0% (95%CI, 12.8% to 96.1%), respectively (Fig. 1E& 1F). We detected 30 mutants in 17 of 58 leukemia driver genes at the timepoint of enrollment. The median mutation number/patient was 1.50 (range, 0-4), and 17 of 20 (85.0%) patients had more than one mutation (≥1) (Fig. 1G). The most frequently mutated genes were FLT3 (ITD/TKD) (20.0%), KIT (15.0%), NRAS (15.0%), and DNMT3A (15.0%) (Fig. 1G). More than half of the patients (11/20) harbored the mutated genes involved in signal transducers (FLT3, KRAS,NRAS, KIT, PTPN11, CSF3R; 11/20, 55.0%), and all these patients achieved CR/CRi (11/11, 100%) after induction therapy (Fig 1G). It is worth noticing that, we observed a high mutant's clearance with VAF (variant allele frequency) dramatical reduction (to <0.01%) (Fig. 1H) after the induction therapy, indicating that mutations involved in signal transducers were rapidly and significantly associated with high clinical response. We also identified 2 patients with MLL-AF9 and 4 patients with CBF-β-MYH11. Both patients with MLL-AF9 reached complete molecular remission (<0.1%) after induction. 3 of 4 patients with CBF-β -MYH11 reached complete molecular remission (<0.1%), and the expression level of the CBF-β -MYH11 fusion gene in 1 patient decreased over 1000-fold at the molecular level (512.16% to 0.28%) after 1 cycle of induction. The MRD negative was 84.2% (16/19) in patients who reached CR/CRi after the 1st cycle of induction therapy (Fig. 1I, 1J). Also, MRD were negative in all 3 patients with favorable risk, 77.8% with intermediate-risk, and 87.5% with poor-risk (Fig. 1K). Infection (grade 1-4) was the most common non-hematological AE (65.0%). Other AEs of grade 3 or higher included fatigue (5.0%), decreased appetite (5.0%), and hepatic dysfunction (5.0%). The most common grade 3-4 hematological AEs were neutropenia and thrombocytopenia. The median duration of neutropenia and thrombocytopenia were 12d (IQR, 11 to 15) and 14d (IQR, 12 to 16), respectively. No patients discontinued the induction treatment and no patient died within 8 weeks of the treatment.
Conclusion This trial demonstrated that the adding of Aza to HIA/HDA regimen is an effective first-line therapy for previously untreated young or fit AML patients, with high efficacy and well tolerance. This study provides preliminary results for the clinical application of this novel combination therapy.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal